This article has been prepared to enlighten you about your cataract surgery in general. This pamphlet should address most of your queries. It is not intended to take the place of a discussion with your physician but may serve as a starting point for dialogue. If you have any questions or require more explanations after reading it, please speak with a member of the healthcare team who is caring for you.
The term “cataract” refers to a clouding of the eye.
A cataract develops when the lens of the eye becomes clouded. This occurs normally as you age. Cataracts can occur in younger people as a result of other medical disorders, such as diabetes, or as a result of inflammatory illnesses such as uveitis or lens damage.
Why do you need cataract surgery?
Cataract surgery is often performed to enhance eyesight clarity.
It is no longer essential to wait for the cataract to “ripen” due to the advancement of current surgical methods. Cataract surgery can be performed at any time, but it must clearly be worth the small percentage risk. In other words, the treatment will be performed if it would have a negative impact on your lifestyle. This is dependent on how you believe the surgery affects your eyesight and on the advice of your expert regarding the treatment’s hazards.
Additionally, you will be told if you have any additional eye disorders that may impair the outcome of the procedure or make it somewhat more hazardous. You’re less likely to require spectacles for distant vision and may simply require reading glasses.
How is a cataract surgery carried out?
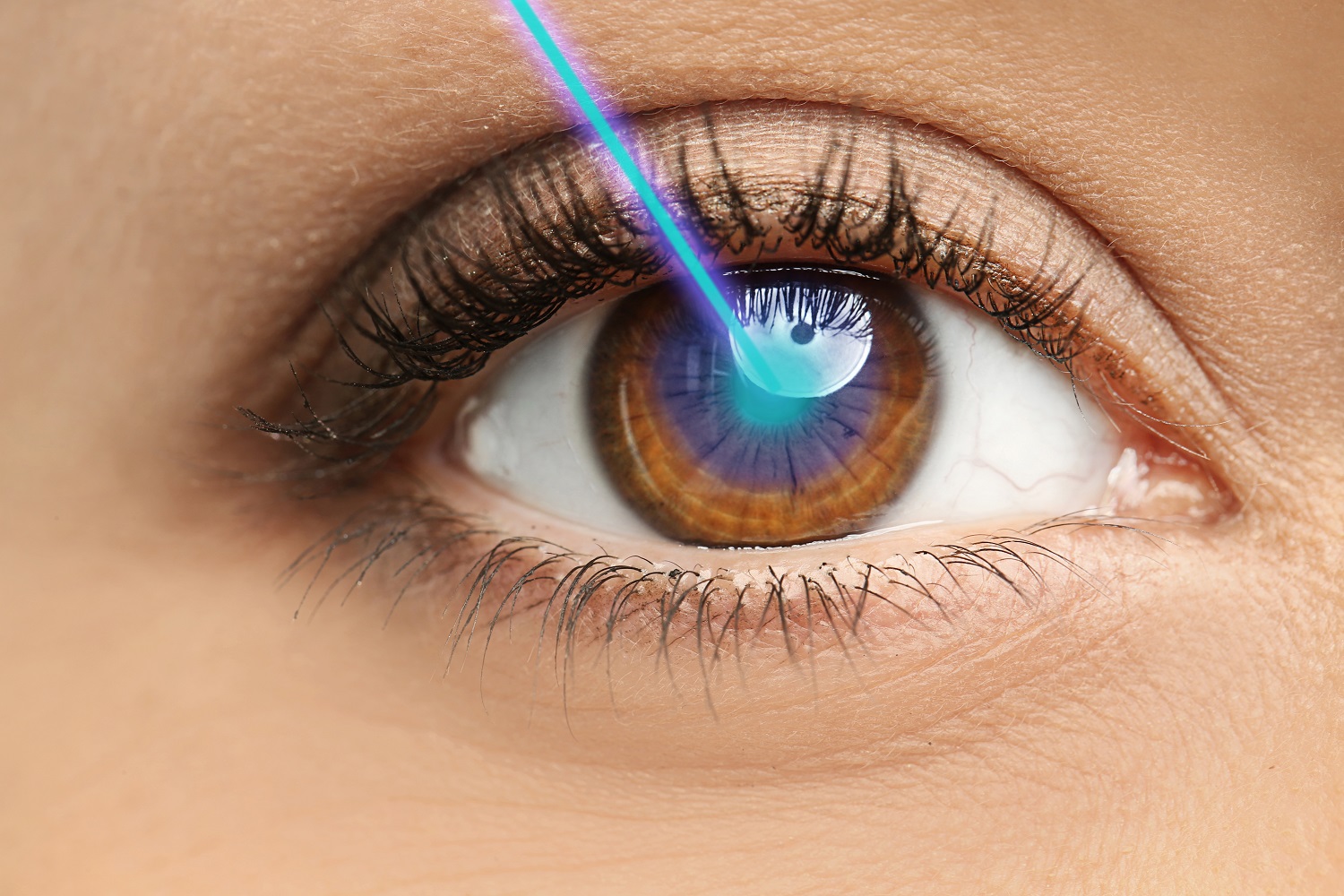
A vibrating needle and a stream of fluid are used to remove the cataract; this treatment is termed phacoemulsification. This is the safest procedure available at the moment since the little incision closes quickly and seldom requires sutures. We employ a piece of “state-of-the-art” equipment to remove the cataract. Please keep in mind that we do not remove cataracts using a laser.

To access the cataract, a tiny incision is made at the edge of the cornea, the eye’s clear window. The cataract’s membranes are retained in order to secure the implant in place. After the hazy substances are removed, this membrane becomes transparent. Unfortunately, the membranes have a propensity to get hazy with time. When a perspex implant is utilized, the likelihood of this occurring is around 50% after five years. However, we choose acrylic or silicone implants since they have been found to have a significantly reduced risk of opacification (cloudiness) – between 5% and 30% within five years. If membrane opacification does occur, simple outpatient laser surgery can be performed to restore vision.
Do I require glasses following cataract surgery?
The majority of people will continue to require glasses following cataract surgery.
Artificial intraocular lens implants (IOLs) are available in a variety of strengths (powers), and the surgeon can select an IOL that improves your focus for distant or near vision.
In the majority of instances, an IOL with adequate distance vision will be implanted to reduce your reliance on spectacles for distance vision. You will use glasses mostly for reading, but you may also want glasses for fine distance focusing.
Certain individuals may choose to have good near eyesight without glasses (for reading or for detailed close work such as embroidery). If you select this route, you will mostly require distance glasses. This is a possibility that you may explore with your surgeon at your cataract assessment clinic appointment.
Multifocal intraocular lenses (IOLs) are lenses that try to correct vision for both distance and near, allowing you to be virtually spectacle-free; however, they are not covered by the NHS.
Are there any possible drawbacks or risks?
As with any operation, there are some minor risks. Although problems from cataract surgery are uncommon, they can be quite significant, with potentially life-changing consequences, and we feel obligated to disclose them with you. The majority of surgical problems may be properly treated. All of these issues might result in a delay in your eye’s healing. You may require more procedures or therapy and may need to schedule additional follow-up sessions. In rare instances, you may require hospitalization to manage problems.
The chance of losing sight or even an eye following cataract surgery has been estimated to be less than 0.03 percent.
You may feel certain that we will not contemplate cataract surgery for your eye unless we have discussed the risks and benefits with you. At the pre-operative evaluation clinic, we will explain any extra risks that may apply to your circumstance. In view of these hazards, cataract surgery should not be approached lightly. This is not an “easy procedure.” It is a significant procedure on the eye.
The dangers and consequences of cataract surgery are discussed in depth here.
Throughout the cataract surgery
• Typically, during the cataract surgery procedure, the implant (intraocular lens) is placed on the membrane that was affected by the cataract (called the posterior capsule). A hole may develop in this membrane for a variety of causes (posterior capsule rupture), which may result in further difficulties. It may be essential to reposition the implant within the eye or to postpone implant placement until a later date.
• If a hole develops in the capsule, vitreous humor (the gel that fills the back of the eye) may escape, increasing the risk of retinal detachment and necessitating further surgical maneuvers, either during the cataract procedure or at a later date.
• Another risk associated with posterior capsule rupture is that a portion of the cataract, or the entire cataract, may fall into the back half of the eye. This problem needs further specialized surgery. This might be accomplished immediately or within a few days.
• Bleeding within the eye can occur during cataract surgery, which might result in vision loss.
• Additionally, local anesthetic operations might result in bruising behind the eye. This can cause the procedure to be delayed or perhaps result in vision loss owing to strain on the ocular nerve.
• While the majority of cataract surgeries are performed with a tiny incision, some must be “converted” to a bigger wound method owing to technical issues during surgery. Occasionally, your surgeon will determine from the start that the bigger wound method is the best option for your eye condition. Visual outcomes one year after surgery are remarkably comparable across the procedures, according to studies. • Although stitches are not usually used on larger wounds, they may need to be removed or altered during the post-operative period.
• Although minor incisions are not sewn, one or two stitches may be applied to a small wound if necessary during the procedure. Typically, these sutures may be removed shortly after the operation (a painless outpatient procedure).